Meniscus Tear- Knee Injury
Meniscus Tear- Knee Injury
Anatomy
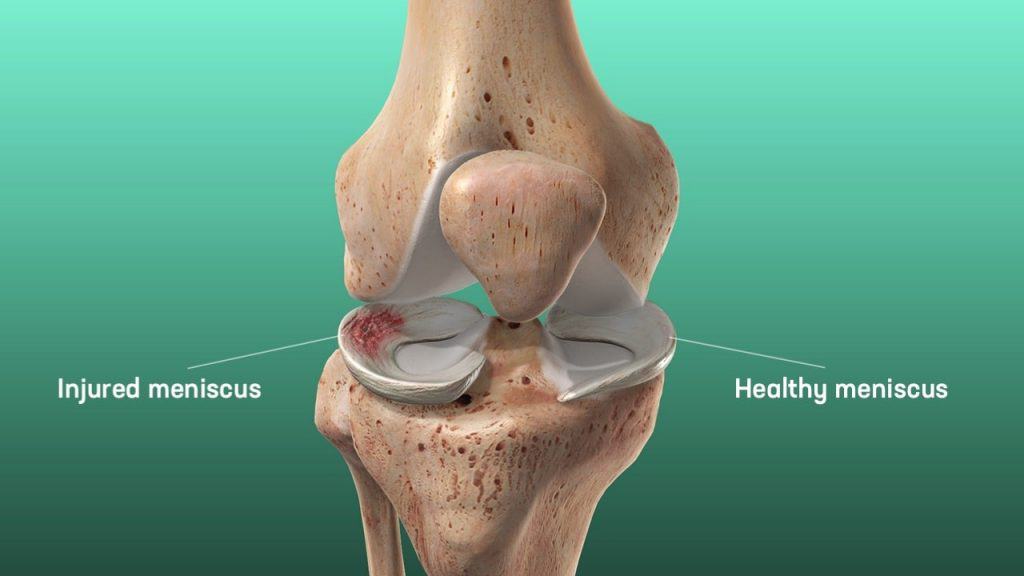
There are two menisci in knee joint. The lateral meniscus is smaller, circular and “O-shaped”. The medial meniscus is C-shaped, broader, but thinner than the lateral meniscus with a flat under surface. Medial meniscus is much broader posteriorly than in anterior aspect and is attached firmly to the medial articular surface of the tibia, joint capsule and tibial collateral ligament at the circumference by coronary ligaments.
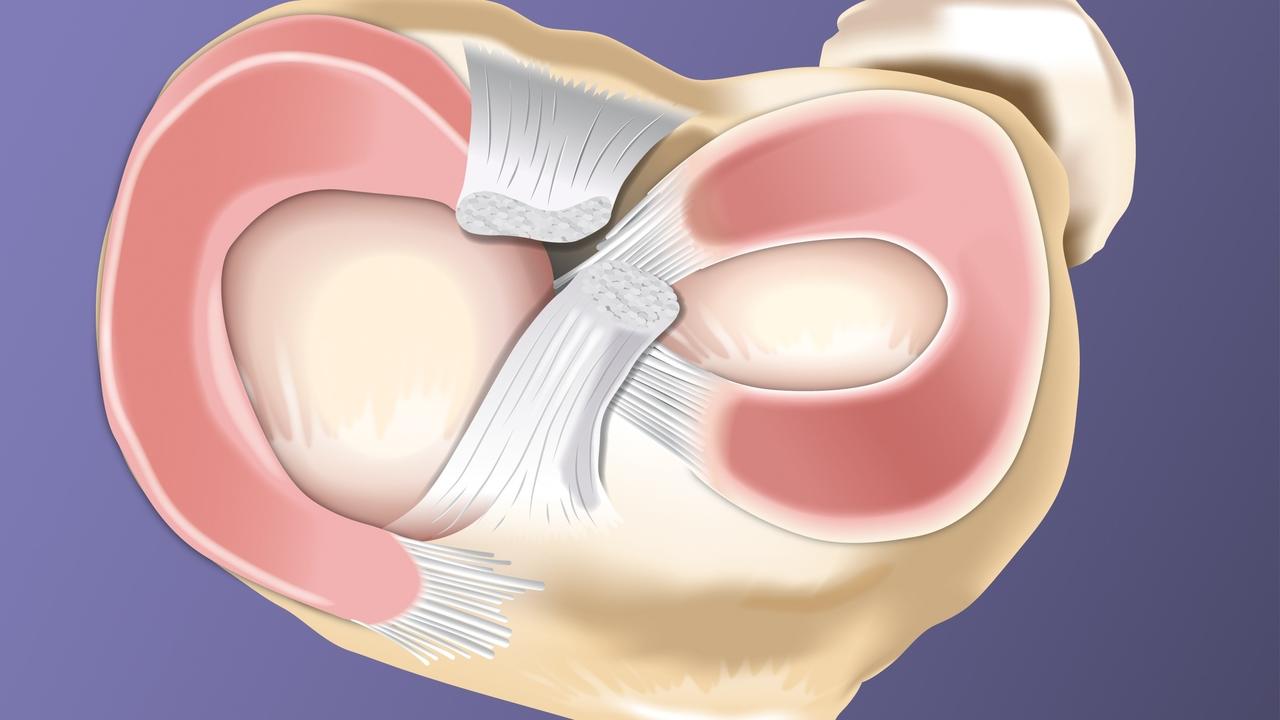
The lateral meniscus is loosely attached to the articular surface of tibia and lateral joint capsule. Posteriorly, it is attached to popliteus tendon. Its anterior attachment merges with the insertion of the ACL. Anteriorly, the two menisci are connected by transverse ligament in front of ACL.
Functions
- Load distribution:
The meniscus functions to optimize force transmission across the knee. It does this by increasing congruency which increases contact area and leads to even distribution of weight load.
- shock-absorption:
the meniscus is more elastic than articular cartilage, this property helps in absorption of shock transmits 50% weight-bearing load in extension, 85% in flexion.
- Stability:
the meniscus increases depth of tibial articular surface and acts as secondary stabilizer. Posterior horn of medial meniscus is the main secondary stabilizer to anterior translation of tibia. It is very important particularly after ACL tear as it is the only primary stabilizers in the ACL-deficient knee.
Etiology
Meniscal tears are common sports-related injuries in young athletes and can also present as a degenerative condition in older patients.
Medial meniscal tears are more common than lateral tears. The exception is in the presence of an acute ACL tear, lateral tears are more common.
Degenerative tears which are common in older patients usually occur in the posterior horn of medial meniscus
The most common mechanism is rotatory force at the knee in either extended or flexed position when it is bearing weight.
The second common mechanism is deceleration or acceleration with direction change as in a cutting motion while running.
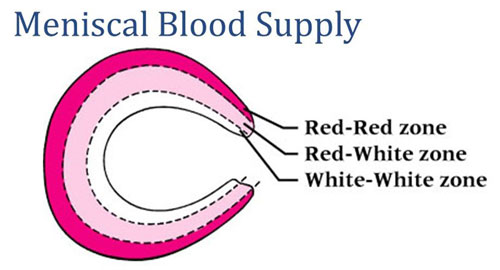
Zones of Meniscus
- red zone (outer third, vascularized) – has good healing potential
- red-white zone (middle third)–moderate healing potential
- white zone (inner third, avascular) – Poor healing potential
Types of meniscal tear
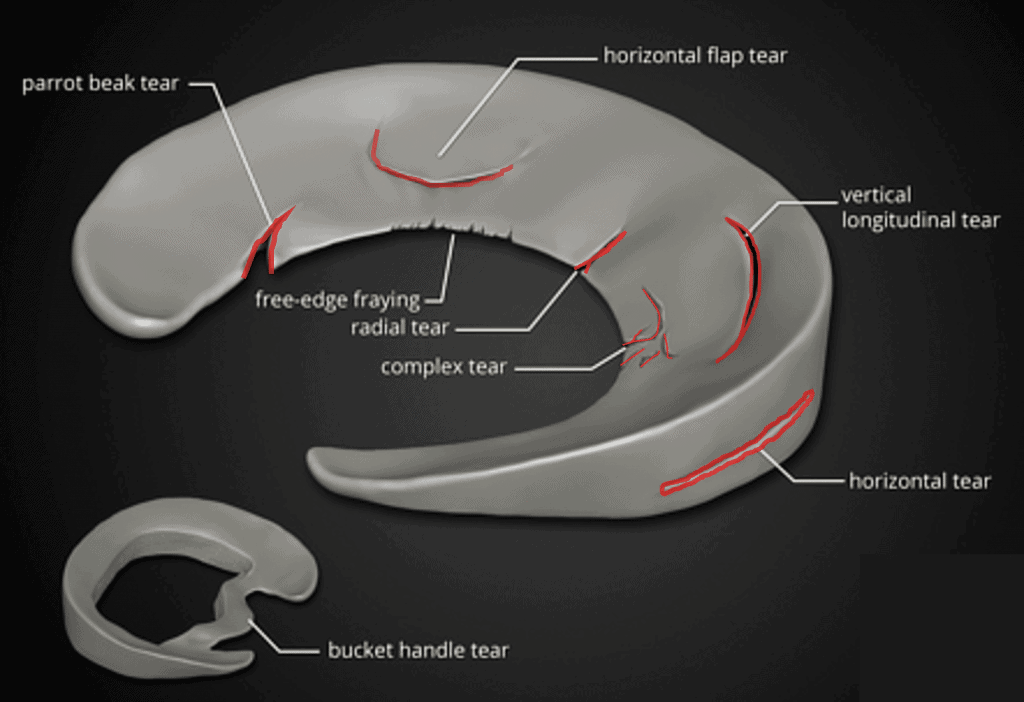
- vertical/longitudinal tear – most common type, especially seen with ACL tears.
- bucket handle tear – seen when vertical tear which may displace into the notch.
- Oblique/flap/parrot beak tears -may cause mechanical locking symptoms
- Radial tears
- Horizontal tears – more common in older population, may be associated with meniscal cysts
- Complex tears
- Root – functionally equivalent to a total meniscectomy, always needs surgery.
- Lateral root tears associated with ACL tear
- medial root tears associated with chondral injuries
Presentation:
Symptoms:
- pain localizing to medial or lateral side of joint line.
- mechanical symptoms (locking and clicking), especially with squatting
- delayed or intermittent swelling
Physical examination:
- joint line tenderness is the most sensitive physical examination finding
- mild to moderate joint effusion may be seen.
Provocative tests to detect meniscal tears
Apley compression test –
With the patient prone, the knee is flexed to 90 degrees and the anterior thigh is fixed against the examining table. The foot and leg are then pulled upward to distract the joint and rotated to place rotational strain on the ligaments; when ligaments have been torn, this part of the test usually is painful. Next, with the knee in the same position, the foot and leg are pressed downward and rotated as the joint is slowly flexed and extended; when a meniscus has been torn, popping and pain localized to the joint line may be noted. Although the McMurray, Apley, and other tests cannot be considered diagnostic, they are useful enough to be included in the routine examination of the knee.
The examiner applies distraction force to the leg to separate the tibia and femur and moves it back and forth. If the capsule or ligaments are injured pain will occur. This test distinguishes if the pain in knee is coming from meniscus injury or extra-articular structures. Torn meniscus pain will be relieved in distraction test. Next, the examiner applies compression and repeats the maneuver if the pain is due to meniscus tear, then distraction test will be negative while pain will occur on compression test.


The McMurray test
With the patient supine and the knee acutely and forcibly flexed, the examiner can check the medial meniscus by palpating the posteromedial margin of the joint with one hand while grasping the foot with the other hand. Keeping the knee completely flexed, the leg is externally rotated as far as possible and then the knee is slowly extended. As the femur passes over a tear in the meniscus, a click may be heard or felt.
The lateral meniscus is checked by palpating the posterolateral margin of the joint, internally rotating the leg as far as possible, and slowly extending the knee while listening and feeling for a click.
A click produced by the McMurray test usually is caused by a posterior peripheral tear of the meniscus and occurs between complete flexion of the knee and 90 degrees. Popping, which occurs with greater degrees of extension when it is definitely localized to the joint line, suggests a tear of the middle and anterior portions of the meniscus. The position of the knee when the click occurs thus may help locate the lesion.
A click localized to the joint line is additional evidence that the meniscus is torn; a negative result of the McMurray test does not rule out a tear.

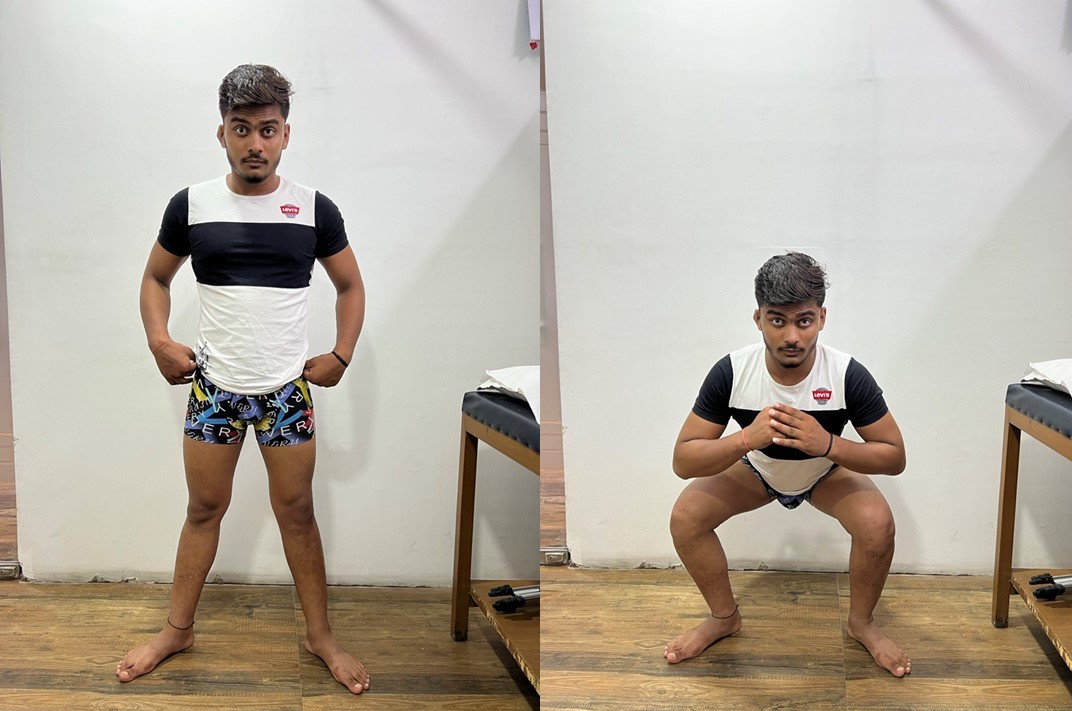
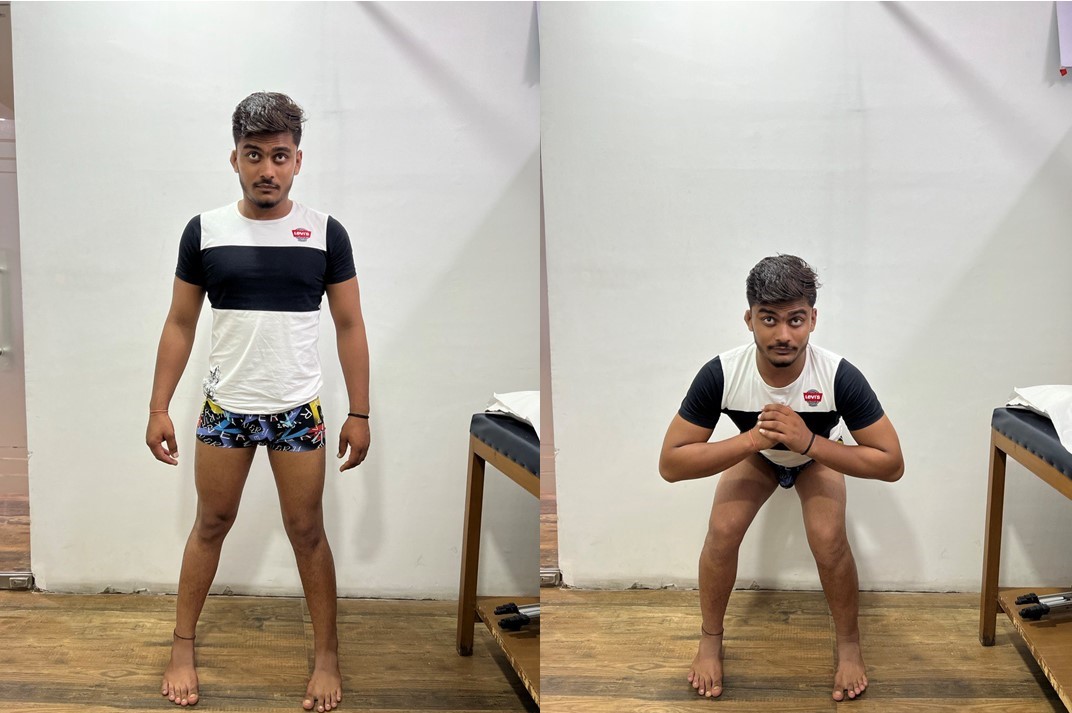
Squat test –
Consists of several repetitions of a full squat with the feet and legs alternately, fully internally and externally rotated as the squat is performed. Pain usually is produced on either the medial or lateral side of the knee, corresponding to the side of the torn meniscus.
Pain in the internally rotated position suggests injury to the lateral meniscus, whereas pain in the external rotation suggests injury to the medial meniscus. The localization of the pain to either the medial joint line or the lateral joint line, however, is a much more dependable localizing sign than the position of rotation.
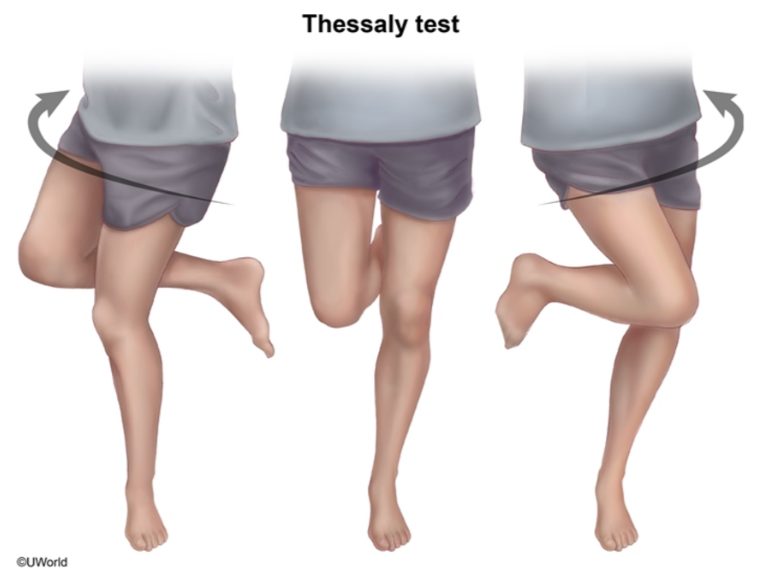
Thessaly test
The examiner supports the patient by holding his or her outstretched hands while the patient stands flatfooted on the floor. The patient then rotates his or her knee and body, internally and externally, three times with the knee in slight flexion (5 degrees). The same procedure is carried out with the knee flexed 20 degrees.
Patients with suspected meniscal tears experience medial or lateral joint-line discomfort and may have a sense of locking or catching. The test is always done on the normal knee first to teach the patient how to keep the knee in 5 and 20 degrees of flexion and how to recognize a possible positive result in the symptomatic knee.
Grading scale for meniscal tears:
- Grade 0 – is a normal meniscus.
- Grade I and Grade II- indicate partial tears that do not involve the free edge.
- Grade III- indicates complete thickness involvement of free edge of the meniscus, indicating a meniscal tear.
Investigations:
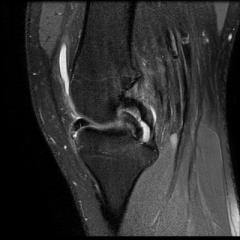
MRI is most sensitive in diagnosing meniscal injury, but it also has a high false positive rate. MRI grade III signal is indicative of a tear is linear high signal that extends to either superior or inferior surface of the meniscus.
Bucket handle meniscal tears may be indicated by “double PCL” sign or “double anterior horn” sign.

Treatment Options:
Nonoperative–
- Rest, NSAIDS, icepack applications followed by rehabilitation
- indicated as first line treatment for degenerative tears, grade I and II tears.
Operative –
Indications:
(1) symptoms of meniscal injury that affect activities of daily living, work, and sports;
(2) positive physical findings of joint line tenderness, joint effusion, limitation of motion, and provocative signs, such as pain with squatting or a positive flexion McMurray or Apley grind test;
(3) failure to respond to nonsurgical treatment, including activity modification, medication, and a rehabilitation program;
a) Partial meniscectomy
Indicated in tears not amenable to repair (complex, degenerative, radial tear patterns), repair failure >2 times. Patients have >80% satisfactory function at short term follow-up. On long term follow –ups, maximum patients will develop osteoarthritic changes and will have Fairbanks radiographic changes (osteophytes, flattening, joint space narrowing).
b) Meniscal repair
I personally believe always an effort should be made to repair the meniscus whenever indicated. Best candidate for repair is a tear with the following characteristics:
- peripheral tears in the red zone (vascularized region)
- vertical and longitudinal meniscal tear heal better than radial, horizontal or degenerative tear
- root tear
- Bucket handle meniscus tear
Bucket handle meniscal tears can be diagnosed on MRI as a double PCL sign on sagittal imaging. These should be repaired in order to preserve meniscal biomechanics and protect from future chondral injury. Following reduction of the meniscal tear, one of a variety of fixation techniques should be used to secure the large flap of the meniscus. The various methods include inside-out (gold standard), outside-in, and all inside techniques. Recent studies have shown the three techniques to lead to equivalent outcomes.
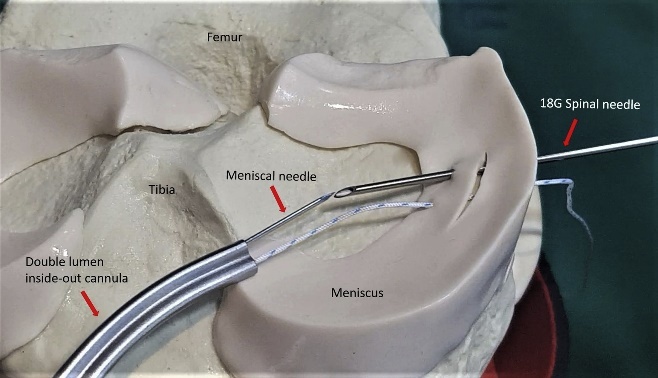
At present, there are three main techniques for meniscal repair: inside-out, outside-in, all-inside.
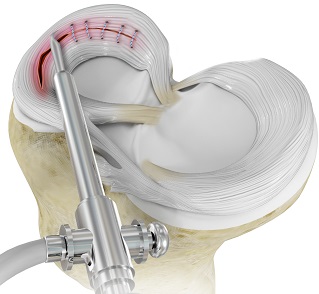
Among them the strongest repair has been accepted as the inside-out technique. In this technique, the tear is fixed by placement and fixation of the passing sutures from the intra-articular region with the use of special cannula to a safe extracapsular area over the capsule with a posterolateral or posteromedial incision.
Outside-in technique is less frequently used, passing sutures were passed through the previously passed two spinal needles from the meniscal rim to the meniscal body across the meniscal tear. The two ends of the passing sutures were tied onto the capsule, under direct vision.
All inside meniscal repair is latest and trending technique, it uses special preloaded sutures and does not require additional posterolateral or posteromedial incision. Results are comparable with inside out technique and cosmetically well acceptable
c) Meniscal repair combined with ACL reconstruction-
traditional literature report higher healing rates with concurrent ACL reconstruction.
modest result when done with an intact ACL (60%)
poor results with untreated ACL-deficiency (30%)
d) Meniscal transplantation
indicated in young patients with near-total meniscectomy, especially lateral tears.
Contraindications are – inflammatory arthritis, instability, marked obesity, grade III and IV chondral changes. malalignment (if not concurrently addressed), diffuse arthritis.
It requires 8-12 months for graft to fully heal and return to sports by 12 – 14 months
e) Total meniscectomy
This of historical interest only, not being performed now a days. Severity of degenerative changes is proportional to percentage of the meniscus that was removed.
Our Result


