MPFL Injury
MPFL Injury
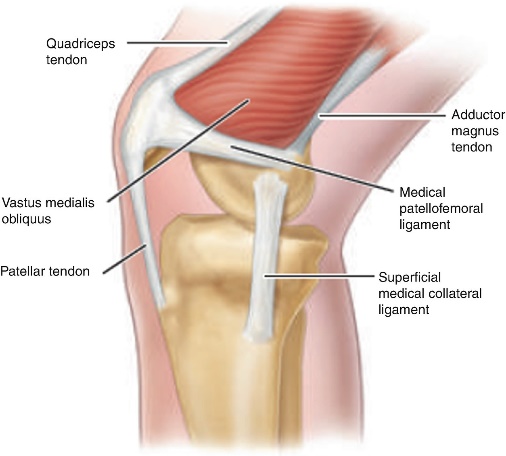
MPFL stands for medial patellofemoral ligament. This is a part of the complex network of soft tissues that stabilize the knee. The MPFL attaches the inside part of the patella (kneecap) to the long bone of the thigh, also called the femur. The MPFL plays a major role in the stabilization of the medial aspect of the patella. It acts in maintaining appropriate patellar tracking within the trochlear groove, while providing 50-60% of the restraining force against lateral displacement, particularly during the early knee flexion between 0 – 30 degrees. It originates from the adductor tubercle to insert onto the superomedial border of the patella.
Risk factors
- Congenital ligamentous laxity
- Miserable malalignment syndrome: includes 3 anatomic characteristics that lead to an increased Q angle, femoral anteversion, genu valgum.
- external tibial torsion / pronated feet
- Patella alta: high riding patella results in misarticulation with sulcus, losing its constraint effects
- trochlear dysplasia
- excessive lateral patellar tilt
- lateral femoral condyle hypoplasia
- Dysplastic vastus medialis oblique (VMO) muscle
- Overpull of lateral structures
Etiology
Usually occurs due to noncontact twisting injury with the knee extended and foot externally rotated. Patient will usually forcefully contract quadriceps thereby reducing the patella, which may result in osteochondral fractures that occur during patellar relocation.
Direct blow on medial side of patella with knee in initial stage of flexion, example: knee to knee collision in basketball, or football helmet to side of knee.
Symptoms
- Complaints of instability
- Anterior knee pain
- Patient complains of lack of confidence during activities like stair climbing, running etc.
- In acute cases tenderness present on medial side of patella.
Physical examination
- Acute dislocation usually associated with a large hemarthrosis
- Absence of swelling may indicate ligamentous laxity and habitual dislocation
- Medial sided tenderness over patella
- Increased passive lateral patellar translation– amount of lateral translation should always be compared to contralateral side.
- Patellar apprehension test is positive
- Increased Q angle, patella alta, osseous anomalies need to be excluded
Imaging
Radiographs
Recommended views of the knee, AP, lateral and axial views
AP view – joint alignment, fracture, knee arthritis can be confirmed
lateral view – to confirm patella alta vs baja, femoral condyle dysplasia
axial view – patellar malalignment, trochlear groove depth, arthritis, vertical patellar fracture
CT
Not used routinely, gives better visualization of the patellofemoral joint alignment.
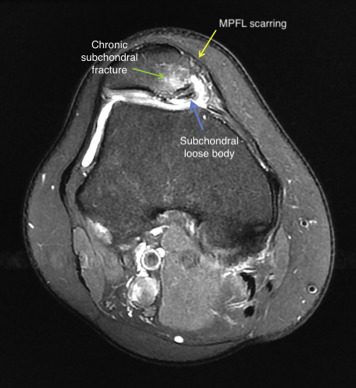
MRI
Best modality to confirm MPFL tears, assessment of articular cartilage and chondromalacia can be done. We recommend 3 tesla MRI for sports injuries as it give better visualisation of small structures.
Treatment Options
- Nonoperative
It is the mainstay of treatment for the patients with first time patellar dislocation without any loose bodies or intraarticular damage and partial MPFL tear.
It includes rest, icepack applications, anti-inflammatory drugs, activity modifications and physiotherapy.
Short-term immobilization for comfort followed by 6 weeks of controlled motion, closed chain short arc quadriceps exercises, Quad strengthening, core and hip strengthening to improve limb positioning and balance, patellar stabilizing sleeve or “J” brace may be beneficial.
- Operative treatment
MPFL repair:
Indicated in acute first-time dislocation with bony fragment. Any patient with MPFL tear and instability needs surgery. This surgery is performed during initial days of injury. It is not preferred in older injuries because of increased failure rates.
Fiber Tape internal brace Augmentation Repair of MPFL:
We believe, by using Fiber Tape augmentation as an Internal Brace during MPFL tear can prevent lateral patellar translation, the MPFL will have a better chance of healing primarily and repair of any concomitant cartilage lesions is protected from additional instability episodes after surgery. Additionally, the MPFL augmentation repair can be performed in a minimally invasive manner and without the need for tendon autograft or allograft.
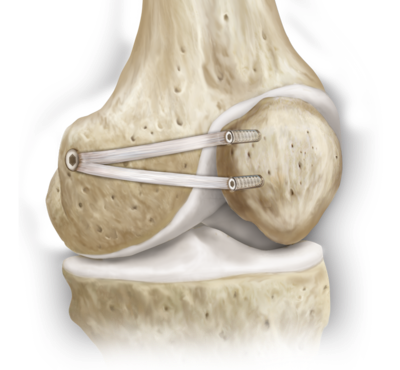
MPFL reconstruction with autograft
Indicated in complete MPFL tear, partial tears with recurrent instability and without any significant underlying malalignment. We use one hamstring graft to reconstruct your MPFL.
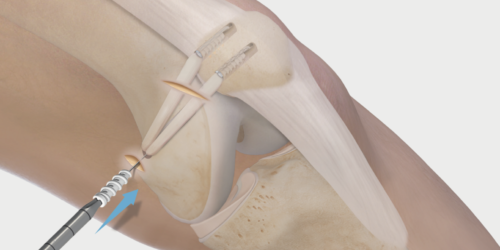
MPFL reconstruction with autograft and Fiber Tape internal brace Augmentation
It is done under regional anaesthesia, which makes it a painless procedure. Patient will be awake during this procedure. MPFL reconstruction performed using hamstring graft and FiberTape augmentation. FiberTape gives extra protection and allows good healing graft which ensures early return to sports.
Our Result


