Shoulder Dislocation and Bankart Tear
Recurrent of Shoulder Dislocation and Bankart Tear
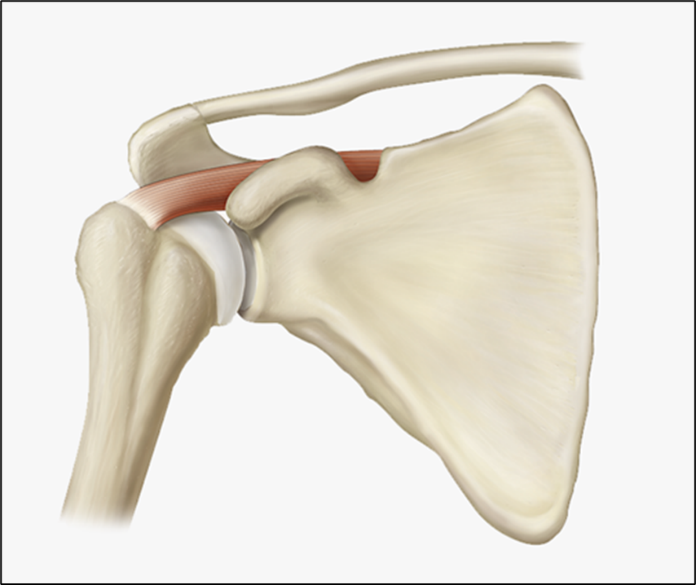
The shoulder joint is a ball and socket type of joint. This is formed by the head of the humerus, which is the ball of the jointand glenoid cavity, which is the socket of the joint. It is one of the most mobile joints in the human body. This hyper mobility makes shoulder joint most unstable joint of the body.
Stability of shoulder joint is provided by 2 types of stabilizers.
- Static stabilizers
- Dynamic stabilizers
Static stabilizers are-
- Glenohumeral ligaments
- Glenoid labrum
- Articular congruity and version
- Negative intraarticular pressure
- Joint capsule
- Rotator interval
Dynamic restraints-
Glenohumeral ligaments – These are the primary stabilizers of shoulder joint.
- SGHL –
Arises from anterosuperior glenoid labrum and superior glenoid tubercle (12 – 1 o’ clock position) to medial ridge of intertubercular groove on humerus. It is the primary restraint to inferior translation at 0° degrees of abduction (neutral rotation)
- MGHL –
Arises from 2 to 3 o’clock position and inserts on the anatomical neck, medial to the lesser tuberosity. It limits the external rotation and anterior translation of the humeral head with the arm in midrange of abduction (45° of abduction).
- IGHL – it has 2 Bands –
Anterior band IGHL
It anchors into anterior labrum and forms weak link that predisposes to Bankart lesions. It is primary restraint to anterior/inferior translation 90° abduction and maximum ER (late cocking phase of throwing.)
Posterior band IGHL
It is the most important restraint to posterior subluxation at 90° flexion, adduction and IR.
Tightness leads to internal impingement and increased shear forces on superior labrum – Glenohumeral internal rotation deficit (linked to SLAP lesions)
Glenoid labrum
Helps to create cavity-compression and increases 50% of the glenoid socket depth, increases the surface contact area with the humeral head. The glenoid labrum acts as a chock-block or wedge to prevent the humeral head from rolling off the glenoid and acts as a static stabilizer through a buttress effect. This is the attachment site for the shoulder capsule, glenohumeral ligaments, and long head of the biceps tendon.
anterior labrum – anchors IGHL (weak link that leads to Bankart lesion)
superior labrum – anchors biceps tendon (weak link that leads to SLAP lesion)
Articular congruity and version
Ball and socket articular configuration help in maintaining stability.
Negative intraarticular pressure
Negative intra-articular pressure aids in centering the head; this is enhanced by “suction cup” effect of labrum. It stabilizes joint, any fall in pressure results in joint to dislocate inferiorly.
Joint capsule
Acts as soft tissue static stabilizer
Rotator Interval
Includes the capsule, SGHL, coracohumeral ligament and long head biceps tendon that bridge the gap between the supraspinatus and the subscapularis.
Boundaries –
- medially by lateral coracoid base
- superiorly by anterior edge of supraspinatus
- inferiorly by superior border of subscapularis
- lateral apex formed by transverse humeral ligament
contracture of the rotator interval is seen with adhesive capsulitis (frozen shoulder)
laxity of the rotator interval results in a visible sulcus sign with inferior laxity with the shoulder in adduction
Biceps Long Head(dynamic)
Long head of biceps acts as humeral head depressor. It has variable origin from superior labrum and forms weak links that predisposes to SLAP tear.
Rotator cuff muscles
The primary biochemical role of the rotator cuff is stabilizing glenohumeral joint by compressing the humeral head against the glenoid.
Shoulder Instability is divided asfollows:
- Unidirectional: Anterior, posterior, inferior or superior.
- Multidirectional:
- With primary structural changes
- Without structural changes but with muscular dyskinesia.
ANTERIOR INSTABILITY AND BANKART TEAR
It is one of most common shoulder injuries. It has a high recurrence rate that correlates with age of first episode of dislocation. Usually affected patients 80-90% are teenagers (90% chance for recurrence in age <20). Younger the age more the chances of dislocations.
Mechanism
Anteriorly directed force on the arm when the shoulder is abducted and externally rotated.
Pathophysiology
The anterior band of the inferior glenohumeral ligament (IGHL) is the primary stabilizer that limits anteriortranslation in 90° of abduction. Detachment of this intraarticular ligamentfrom the anterior glenoid rim as the typical lesion found inrecurrent anterior dislocation.
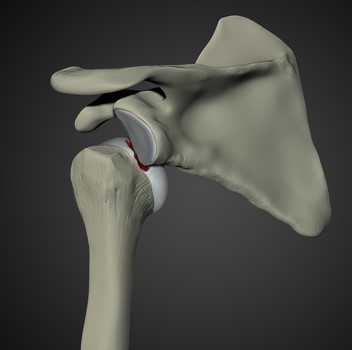
Bankart lesion
It is an avulsion of the anterior labrum and anterior band of the IGHL from the anterior inferior glenoid.

Most common type of injury. The Bankart’s lesion is seen in 87–100% of initial dislocation.
This results in loss of the normal chock-block effect of the labrum, affects the concavity compression mechanism of the rotator cuff, and disrupts the continuity of the inferior glenohumeral ligament.
The glenoid labrum acts as a chock-block or wedge to prevent the humeral head from rolling off the glenoid. In order for a soft-tissue Bankart lesion to occur, the humerus must translate over the wedge of the anterior glenoid.
The Bony Bankart lesion
A piece of glenoid fractures along with the ligamento-labrocapsular complex called the glenolabral articular disruption.
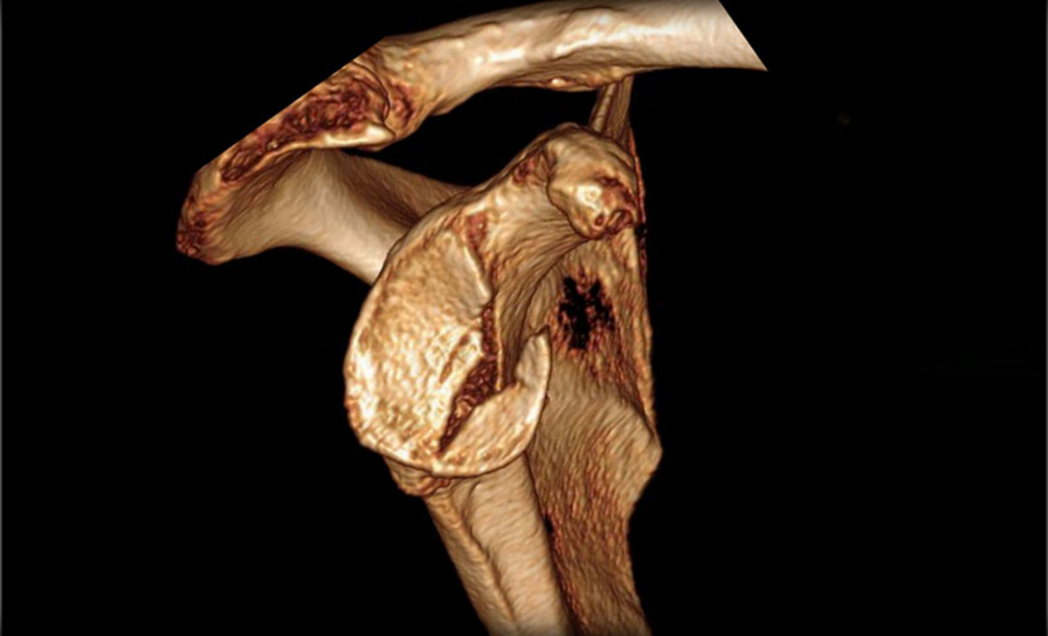
Fracture of the anterior inferior glenoid presents in upto 49% of patients with recurrent dislocations.
Defect >20-25% is considered “critical bone loss” and is biomechanically highly unstable stability cannot be restored with soft tissue stabilization alone (unacceptable >2/3 failure rate) require bony procedure to restore bone loss (Latarjet-Bristow, other sources of autograft or allograft)
Hill Sachs lesion
It is the impaction fracture of the back portion of the top of arm bone occurred during event of dislocation.
The characteristics that increase chances of a dislocation are:
Young age at first dislocation (< 20 years)
Ease of dislocation with applied force (laxity)
Presence of associated lesions as described above.
Anteroposterior Translation Grading Scheme
Grade 0 Normal glenohumeral translation
Grade 1 Humeral head translation up to glenoid rim
Grade 2 Humeral head translation over glenoid rim with spontaneous reduction once force withdrawn
Grade 3 Humeral head translation over glenoid rim with locking
Presentation – Symptoms
Traumatic event causing dislocation
Feeling of instability
Shoulder pain – caused by subluxation and excessive translation of the humeral head on the glenoid
Patient hesitates to abduct and external rotate the shoulder.
Recurrent Shoulder Instability
The complaint of a recurrent dislocation is usually of the shoulder “slipping” or “popping out” during overheadactivities, especially external rotation and extension.
Patient with recurrent subluxation describes a sudden catch, followed by sudden inability to move the arm with a “numb” feeling the so-called “dead arm syndrome” (the feeling of dead arm syndrome can also arise in SLAP lesion).
Most patients are athletic adolescents or young adults with joint laxity. Such individuals may have pain with overhead movements due to an inability to control their laxity by means of their muscles.
The most common presenting complaint is pain. Loss of internal rotation in young patients may be an important finding suggestive of posterior capsular contracture that is often associated with subtle instability.
Physical examination
LOAD AND SHIFT TEST
Patient is sitting – examiner stands posterior to shoulder – with one hand stabilize clavicle and scapula – with the other hand – during load portion of test head is centralized and compressed into glenoid – during shift portion of test head is translated anteriorly and posteriorly noting the amount of force needed to displace the humeral head “out” in anterior and posterior direction.
Grade I – increased translation, no subluxation
Grade II – subluxation of humeral head to, but not over, glenoid rim
Grade III – dislocation of humeral head over glenoid rim
APPREHENSION SIGN
patient supine with arm in 90 abduction and 90 ER position, gradually ER increased with anterior directed force over shoulder. Patients are observed for apprehension – feeling of impending dislocation, more pain is insignificant.
positive sign in mid-ranges of abduction is highly suggestive of concomitant glenoid bone loss
RELOCATION SIGN
Procedure is same as apprehension sign done, then applying a posteriorly directed force on anterior humerus (attempting to reduce anterior subluxation); a decrease in apprehension with a posterior directed force implies anterior instability.

SULCUS SIGN
The sulcus sign signifies anteroinferior labral tear/inferior shoulder laxity/instability. The patient is seated or standing with the arm relaxed by the side. The patient’s arm is grasped by the examiner and pulled inferiorly. Dimpling of the skin below the acromion suggests widening of the subacromial space between the acromion and the humeral head with inferior subluxation of humeral head.
DRAWER TEST
The examiner holds the humeral head while standing behind the patient and pushes forward (for
anterior laxity) and pulls backward (for posterior laxity) inthe glenoid to access translational stability. A clunkor snap on anterior subluxation can suggest Bankart lesion.
INVESTIGATIONS
X-RAYS–
Trauma series x – rays of shoulder – AP, Axillary view and scapular Y view
Helps in diagnosing dislocated joints.
To rule out associated fractures
Axillary view helps in diagnosing REVERSE HILL SACH LESION
Scapular Y-view also helps to evaluate the shape of acromion.
West Point Axillary View helps in accessing anteroinferior glenoid bone loss.
Stryker Notch View – This is very useful for visualization of HILL SACH LESIONS
MRI –
Best for visualization of labral tear. It is most commonly used mode of investigation for labral tear.
MR – ARTHROGRAPHY
Can diagnose a variety of lesions of the shoulder with great accuracy.
Addition of intraarticular contrast increases sensitivity and specificity.
CT – SCAN
It gives better visualization of osseous pathology. Helps in evaluation of bony bankart, Glenoid bone loss, Hill Sach and Reverse Hill Sach lesions.
TREATMENT
Nonoperative
Acute reduction, ± immobilization, followed by physiotherapy
It is done as immediate management if patient comes with dislocated shoulder and done as emergency OPD procedure. Studies have not shown any benefit of immobilization of more than 1 week for decreasing recurrence rates.
Risk factors for re-dislocation are
- age less than 20 years (highest risk)
- male gender
- participation in contact sports
- hyperlaxity of joint
- glenoid bone loss more than 20-25%
Operative
- Arthroscopic Bankart repair +/- capsular shift
Indications
- First-time traumatic shoulder dislocation with Bankart lesion confirmed by MRI in athlete younger than 25 years of age.
- high demand athletes.
- recurrent dislocation/subluxation (> one dislocation) following nonoperative management with less than 20-25% glenoid bone loss.
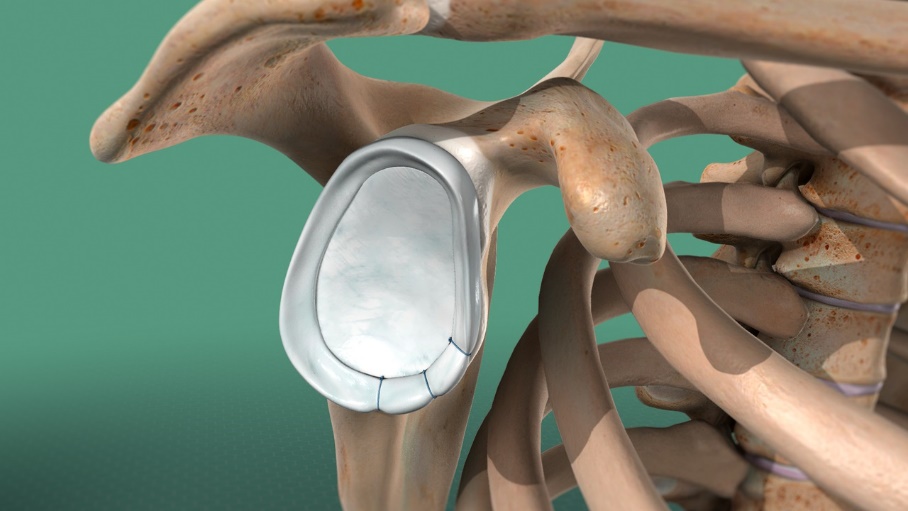
- Open Bankart repair +/- capsular shift
Not preferred now a days because advancement and better results of arthroscopic procedures.
- Arthroscopic Bankart repair with Remplissage
Indications
Engaging large Hill-Sachs defects with less than 20-25% glenoid bone loss.
Technique
Posterior capsule and infraspinatus tendon sutured into the Hill-Sachs lesion
may be performed with concomitant Bankart repair.
- Latarjet (coracoid transfer) and Bristow Procedures for glenoid bone loss
Indications
Chronic bony deficiencies with more than 20-25% glenoid deficiency (inverted pear deformity to glenoid)
Transfer of coracoid bone with attached conjoined tendon and CA ligament
Latarjet triple effect = bony (increases glenoid track), sling (conjoined tendon on top of subscapularis), capsule reconstruction (CA ligament)
Approach – shoulder anterior (deltopectoral) approach
can be performed arthroscopically
.
Our Result


